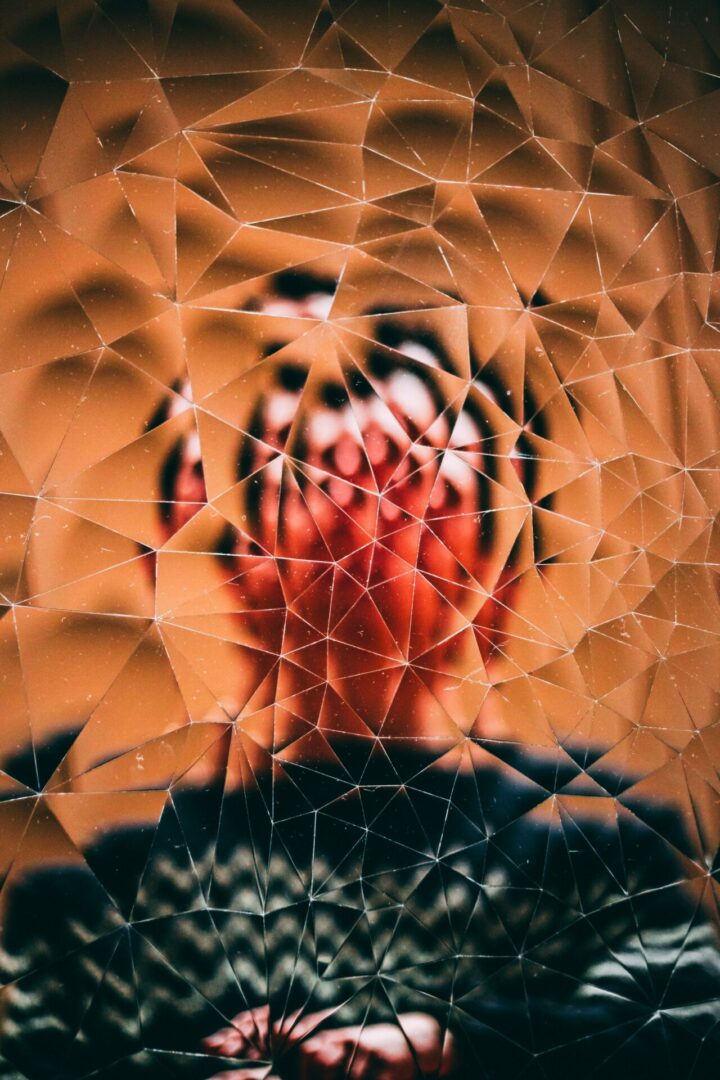
Trauma is not defined solely by what happens to us, but by how our body and nervous system respond to those experiences. It overwhelms our ability to cope, often leaving us in a lasting state of fear, hypervigilance, or numbness. For those recovering from trauma, healing does not begin with revisiting painful memories—it begins with safety.
At Khiron Clinics, we recognise that safety is not just about physical protection. It includes emotional and psychological safety: feeling secure, respected, and connected in a way that allows the nervous system to begin settling. Without this foundation, the body remains in survival mode, making meaningful recovery impossible.
In this article, we explore why safety comes first in trauma recovery, how trauma disrupts that sense of safety, and the ways we support our clients in creating a grounded, safe space—both within themselves and in relationship with others.
What Trauma Does to Our Sense of Safety
Trauma, particularly in childhood, fundamentally disrupts the nervous system and our body’s sense of safety and security (Porges, 2017).
Trauma is the body’s unresolved response to an overwhelming experience that made us feel powerless or trapped. It often occurs when we are unable to fight back, escape, or appease a threat, leaving us frozen, helpless, and vulnerable (Levine, 1997). This freeze response can be triggered by situations ranging from physical entrapment (such as abuse or neglect) to emotional or psychological control, like bullying or manipulation. What causes trauma is not just the event itself, but our inability to act or escape in that moment. Importantly, our response is linked to the ways we have learned to deal with stress since childhood, based on our environment and upbringing. It is highly individual, and never a reflection of your strength or weakness in the face of stress—it is simply a sign of the situations you’ve had to cope with in the past.
For example, people who were exposed to chaos and violence in childhood may cope with feelings of uncertainty and danger in different ways from those raised with stability and consistency.
Similarly, past experiences of trauma affect our perceptions of safety in the present–we respond to situations and stimuli differently based on the fear and lack of safety we have had to cope with in the past. People will often think of examples like small spaces feeling unsafe, touch feeling unsafe, shouting, loud noises, cars and so on. But there are more nuanced examples that can show up in the recovery process. Feeling like your therapist is the one ‘in control’, feeling vulnerable, eye contact, feeling judged, and being asked to recount a traumatic experience can all trigger the fight or flight response, which can leave someone too mobilised to engage, or pass into the freeze response and become too immobilised to engage (Porges, 2011).
The Role of Safety in Effective Trauma Treatment
At Khiron Clinics, we understand that trauma cannot be processed in an environment that feels unsafe—no matter how well-intentioned the treatment. Before any therapeutic work can begin, a foundation of safety must be established. This means not only providing physical safety and consistency, but also cultivating emotional and relational safety, where each client feels seen, heard, and never pressured.
In trauma recovery, the nervous system must feel settled enough to engage. If the body remains in a constant state of survival—hypervigilant, shut down, or dysregulated—then attempts to “talk about” trauma can actually reinforce feelings of helplessness and disconnection. This is why we use bottom-up approaches, working with the body and nervous system while addressing the trauma narrative itself.
Safety in therapy doesn’t mean avoidance. We respect each client’s window of tolerance and respond with interventions that support regulation and connection, not reactivation. These may include somatic practices, grounding exercises, creative expression (like art or movement), and gentle relational attunement. Every step is designed to offer choice, predictability, and control—key elements that help clients rebuild a felt sense of agency (Fisher, 2021).
Ultimately, creating safety is not a one-time task—it is a continuous, dynamic process that forms the heart of trauma-informed care.
Creating Safety: How We Do It, and What Clients Say About Feeling Safe
Creating safety at Khiron Clinics begins with deep respect for each person’s pace, boundaries, and nervous system. We don’t push clients to talk about traumatic experiences before they’re ready. Instead, we focus on building a sense of internal and external safety through routine, choice, and relational consistency.
This includes trauma-informed practices like clear communication, collaboration, and the use of nervous system-informed therapies, such as somatic experiencing, art therapy, breathwork, and body-based approaches that help settle the nervous system. We pay attention to the environment: calm spaces, predictable rhythms, and therapists who are trained to respond with attunement and care. Every part of the therapeutic setting is designed to reduce threat and support nervous system regulation.
Importantly, our clients often share that the safety they feel here is unlike anything they’ve experienced before. As one former client said:
“Even though I couldn’t talk, they found ways to communicate with me, and built up trust over time.”
With another stating:
“For the first time, I was not simply labelled with diagnoses, but treated as an individual”
Moments of felt safety—however small—are powerful. They are the first steps toward healing, and they remind clients that their bodies can relearn what it feels like to be safe, connected, and in control.
Developing A Lifelong Practice of Awareness and Regulation
Safety is not just the starting point of trauma recovery—it’s the ongoing foundation. At Khiron Clinics, we support clients in developing lifelong practices of self-awareness, nervous system regulation, and relational safety. These tools empower individuals to navigate life with greater resilience, connection, and inner stability. Recovery doesn’t happen overnight, but with the right support, it becomes a sustainable path.
If you or a loved one is seeking a trauma-informed space to begin healing, Khiron Clinics is here to help.
References
Fisher, J. (2019). Sensorimotor psychotherapy in the treatment of trauma. Practice Innovations, 4(3), 156–165.
https://doi.org/10.1037/pri0000096
Fisher, J. (2021). Transforming the Living Legacy of Trauma: A Workbook for Survivors and Therapists. PESI Publishing.
Levine, P. A. (2010). In an Unspoken Voice: How the Body Releases Trauma and Restores Goodness. North Atlantic Books.
Levine, P.A. and Frederick, A. (1997) Walking the tiger healing trauma: The innate capacity to transform overwhelming experiences Peter A. Levine Aut; Ann Frederick Aut. Berkeley, Calif: North Atlantic Books.
https://www.somaticexperiencing.com/se-books
Maté, G. (2021). The Myth of Normal: Trauma, Illness and Healing in a Toxic Culture. Random House UK.
https://drgabormate.com/book/the-myth-of-normal/
Porges, S. W. (2011). The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-Regulation. Norton.
https://psycnet.apa.org/record/2011-04659-000
Porges, S.W. (2017) The pocket guide to the polyvagal theory: The transformative power of feeling safe. New York: W.W. Norton.
https://wwnorton.co.uk/books/9780393707878-the-pocket-guide-to-the-polyvagal-theory
Van der Kolk, B. A. (2014). The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma. Viking.
https://www.besselvanderkolk.com/resources/the-body-keeps-the-score